Type 1 Diabetes is an autoimmune disease in which the pancreas stops creating insulin, a hormone needed to break down sugars in your cells. This causes the blood glucose levels to rise severely and remain high, and this could be fatal if left untreated. This condition is usually diagnosed in children or teenagers, and they are left suffering from it for the rest of their lives. There is no outlined known cause for diabetes; the body is said to be triggered by a common virus of bug to start attacking the pancreatic cells. Unlike Type 2, Type One Diabetes isn’t diet related, isn’t preventable and isn’t the diabetics fault. In the last 15 years, the advances in diabetes treatment have been outstanding, but the new types of pumps and continuous glucose monitors don’t to our long awaited cure.
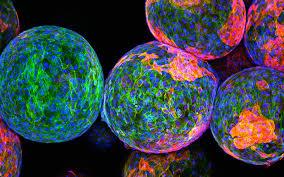
One major part of diabetes cure research is beta cells. These are the cells that actually make the insulin in your pancreas. They are found in clumps of around 100, and these are called islets of Langerhans. In order to research a cure, we need to understand these islets- how they work, grow and how to give new ones to diabetics. Research scientists have already tried implanting beta islets into diabetics, but these people will have to take drugs for the rest of their lives to stop their bodies from rejecting the cells, and we can’t be sure they could work fully so the diabetic would still be slightly insulin dependent. The drugs are uncertain to work anyway, and if you did reject the transplanted cell your body become sick and fight the islets. The risk and downsides of the treatment outweigh the benefits greatly. In response to this however, cure researchers are looking into ways of protecting the beta cells, or new cells that could be fit for transplantation. One way of protecting the cells is encapsulation, which is forming a protective layer around the beta cells before putting them in the body.
In order for implanted beta cells to have a chance at working, a diabetic’s body needs to be trained to not attack these insulin- producing cells. Our immune system mistakenly recognises our beta cells as antigens, which are considers ‘bad’ and then proceeds to fight the cells. To stop this process from happening, we ned to train our immune cells to not do this, by having small, gradual introductions of the cells to stop the attack from happening again. This is much like what is done with food allergies. Researchers are also looking into destroying the actual cells created by the immune system that try to kill the beta cells, to stop the attack in the first place. Scientists like Professor Susan Wong and Gideon Gross are looking into creating ‘assassin cells’ from stem cells that are able to stop these killer immune cells. An even more innovative idea researchers have had is to train diabetic bodies to grow their own beta cells. Because of a breakthrough in 2014, where scientists worked out how to grow their own beta cells from stem cells in a lab, this meant we could study how to keep beta cells alive. It is also possible to use alpha cells, which can be reprogrammed to start creating insulin. these cells make glucagon, and because of the huge similarity between the function and position if the alpha and beta cells, they are easy to 'switch' roles.
In 2016, a trial for new technology called Bio-Inspired artificial Pancreas was tested on a group of 20 people. it is a ‘closed loop’ system, which is connected via a thin tube to the diabetics abdomen, and sends blood glucose levels to an insulin pump which releases the hormone in different amounts when required. It therefore means the diabetic does not need to carry out finger-prick tests, or take injections, and it has been called the best technology on the market5. One of the diabetics testing it said; “Since I’ve been using it my life is 100 times better”. It seems as though, even if we continue searching for the cure, our best efforts should be put into treatments for current and future diabetics. It has been estimated by some experts that it will take up to 25 years to find a cure. The man running the artificial pancreas trial, Dr Nick Oliver, has been quoted to say “There are lots of avenues that will lead to potential cures for Type 1 and Type 2 diabetes and if I could see it in my career that would be incredibly exciting Diabetes can’t be cured at the moment. The race is on to get effective treatments for people. Their quality of life is important.”
by lucy Markham
sutton high school